Address
Australia, Singapore, and USA
Address
Australia, Singapore, and USA

Learn how to secure patient data with HIPAA compliant cloud storage. Our guide covers selecting a provider, key safeguards, and best practices for healthcare.
When you're dealing with patient health records, "just sticking it in the cloud" is a recipe for disaster. That's because standard cloud storage services are built for convenience, not for the ironclad security required by federal law. They're like a basic storage locker—fine for old furniture, but you wouldn't keep priceless jewels in there.
This is where HIPAA-compliant cloud storage comes in. It’s a completely different beast, engineered from the ground up to securely store, manage, and share electronic Protected Health Information (ePHI) according to the strict rules of the Health Insurance Portability and Accountability Act. Think of it as a fortified bank vault, complete with encryption, access controls, and legally-binding agreements designed to protect the most sensitive data imaginable.

If your practice handles patient information, uploading it to a generic cloud drive simply isn’t an option. Regular cloud services lack the specific safeguards needed to protect what the law calls electronic Protected Health Information, or ePHI.
While any cloud service can hold files, a HIPAA-compliant cloud storage solution is built with multiple layers of security designed specifically to meet federal standards. It’s a critical distinction.
To ensure everyone is accountable, HIPAA clearly defines the relationship between two main parties:
This crucial partnership is cemented by a legal document. Without it, you’re breaking the law by using a third-party service for patient data.
The cornerstone of this relationship is the Business Associate Agreement (BAA). This is a legally binding contract that holds your cloud provider accountable. It ensures they will implement specific security measures and accept liability for protecting the ePHI they manage for you. Using a provider without a signed BAA is a direct HIPAA violation.
The Health Insurance Portability and Accountability Act (HIPAA) was passed back in 1996 to set firm standards for patient privacy. As healthcare has gone digital, the need for secure online solutions has exploded. In response, major cloud providers have adapted, adding robust security controls, strong encryption for data both at rest and in transit, and detailed audit logs. For any healthcare organization, mastering these rules is essential for avoiding massive fines and keeping patient trust. You can explore more about the fundamentals of compliant cloud storage for healthcare.
Ultimately, choosing the right storage isn't just a technical decision—it's a core part of patient care. It shows you're committed to protecting the most personal information someone has. This foundational understanding of roles, responsibilities, and specialized solutions is the first step toward building a truly secure and compliant data strategy for your practice.

Trying to make sense of HIPAA regulations can feel like getting lost in a legal maze. The language is dense and intimidating, but the principles at its heart are surprisingly straightforward once you cut through the noise. For any healthcare practice, truly getting a handle on these rules is the first step to choosing a hipaa compliant cloud storage solution that actually protects you.
The HIPAA Security Rule sets the national standards for keeping electronic Protected Health Information (ePHI) safe. It’s not just one big mandate, but a framework built on three distinct pillars called safeguards. Think of them as different layers of defense, all working together to build a fortress around sensitive patient data.
The first pillar, Administrative Safeguards, is all about the human side of security. It covers the policies, procedures, and oversight needed to manage ePHI correctly. This isn't about specific software features; it's about creating a culture of security within your team and expecting the same from your partners.
At its core, this safeguard demands that you perform critical management functions to prevent, detect, contain, and fix security violations.
A huge piece of this is conducting regular Security & Privacy Risk Assessments. This isn't a one-and-done checkbox. It’s a continuous process of looking for weak spots in how you handle data. Where could a breach happen? Who has access to what? Answering these questions honestly is fundamental to staying compliant.
Other key administrative responsibilities include:
The second pillar, Physical Safeguards, deals with the security of the actual, physical hardware where ePHI is stored. This means the servers, computers, and even the buildings that house them. When you team up with a hipaa compliant cloud storage provider, you are essentially outsourcing this massive responsibility to them.
Think of this as the physical security for the bank vault. It involves controlling who can physically get near the servers and protecting them from things like fire, floods, or theft.
A truly compliant cloud provider runs its operations from highly secure data centers. These facilities are fortresses, often featuring multiple layers of security like 24/7 surveillance, biometric scanners, and strict access policies that ensure only authorized staff can ever physically touch the servers storing your patients' data.
These safeguards are non-negotiable requirements. For example, you must have policies for securely getting rid of old hard drives or servers that once held ePHI. You can't just toss them in the dumpster; they have to be physically destroyed or professionally wiped clean to make the data completely unrecoverable.
Finally, we have Technical Safeguards. These are the technologies and related policies that protect and control access to ePHI. If administrative safeguards are the rulebook and physical safeguards are the vault walls, then technical safeguards are the digital locks, keys, and alarm systems.
Two of the most crucial technical safeguards are:
Beyond encryption, this pillar also demands strict access controls. This is about making sure users can only access the absolute minimum information required to do their jobs. Not everyone in your practice needs to see every patient file. A robust system, like the one powering Sky Drive Folder, allows for granular, file-by-file permissions, guaranteeing that sensitive data is seen only by authorized eyes. To see how this works in practice, you can learn more about how permissions are vital to secure document sharing in a regulated environment.
Together, these three safeguards create a comprehensive framework for protecting patient data. Real compliance isn’t about acing one area; it requires constant vigilance across all three—from your internal training to the data centers and encryption protocols of your cloud storage partner.
Choosing the right partner to handle your electronic Protected Health Information (ePHI) is one of the most important decisions you'll make. It’s not about finding a vendor; it’s about finding a true security partner. You have to cut through the marketing noise and focus on what really matters.
The entire process boils down to one simple, non-negotiable question: Will the provider sign a comprehensive Business Associate Agreement (BAA)? If they say no, or offer a flimsy, one-size-fits-all BAA, you should walk away. Immediately. A solid BAA is the legal foundation of your relationship, making the provider liable for protecting the ePHI they manage. Without it, you are simply not compliant.
But signing a BAA is just the price of admission. Real due diligence means digging into the provider's security architecture and how they operate. You need to know exactly how they’ll protect your data, every single day.
A compliant provider can't just give you a vague promise of "security." They need to show you clear, documented proof of their technical and physical safeguards. Your evaluation should be like a thorough inspection of their security engine, focusing on three key areas.
This graphic really highlights the key security features that separate a standard tool from one built for healthcare compliance.
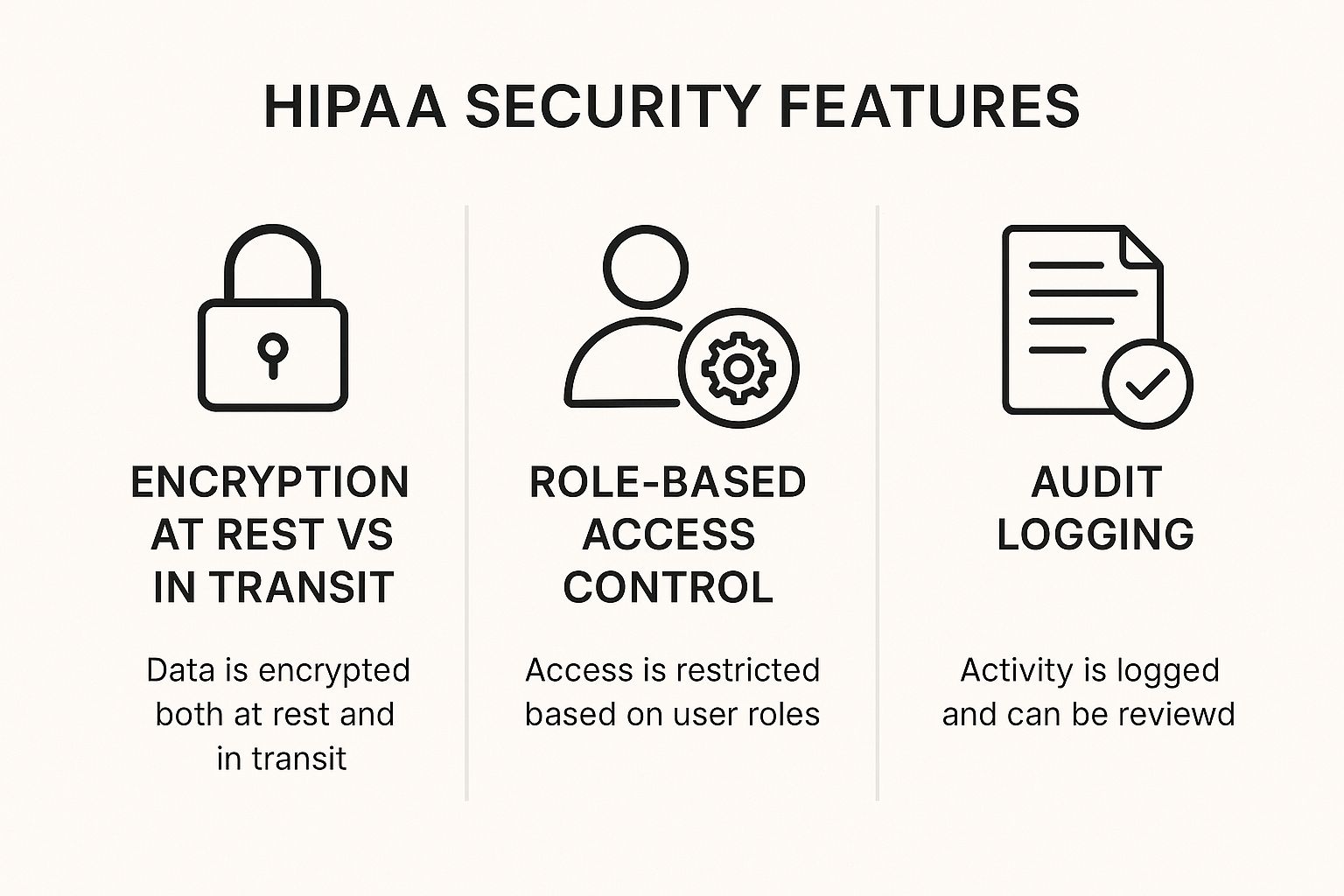
As you can see, features like end-to-end encryption, role-based access, and detailed logging aren't just nice-to-haves. They're foundational parts of any truly compliant system.
Before we go further, it's helpful to see a direct comparison. Here’s how a standard, consumer-grade cloud service stacks up against one designed specifically for HIPAA compliance.
| Feature/Requirement | Standard Cloud Storage | HIPAA Compliant Cloud Storage |
|---|---|---|
| Business Associate Agreement (BAA) | Not typically offered. | Required. A non-negotiable legal contract. |
| Encryption (At-Rest & In-Transit) | Often available, but may not be the default. | Mandatory. End-to-end encryption using strong standards like AES-256 is standard. |
| Access Controls | Basic user permissions (view, edit). | Granular, role-based controls to enforce the principle of least privilege. |
| Audit Trails & Logging | Limited or non-existent activity logs. | Comprehensive audit trails tracking all user actions on ePHI. |
| Data Backup & Recovery | Basic backup, but recovery guarantees are rare. | Documented disaster recovery plans with defined recovery objectives. |
| Data Disposal/Deletion | Files are often recoverable or not permanently deleted. | Secure data disposal methods to permanently destroy ePHI. |
| Shared Responsibility | The user is almost entirely responsible for security. | A clearly defined model where the provider secures the infrastructure. |
This table makes it clear: while both types of services store files, only one is built with the safeguards, legal agreements, and accountability required to protect patient data.
A dangerous misconception is that hiring a compliant provider means you can wash your hands of all security duties. That's completely wrong. HIPAA compliance works on a Shared Responsibility Model, a critical concept that defines who is accountable for what.
Think of it like renting space in a high-security building. The building owner (the cloud provider) is responsible for the building's perimeter security—the locks on the main doors, the surveillance cameras, and the reinforced walls. This is security of the cloud.
But you, the covered entity, are responsible for what happens inside your own office. You decide who gets keys, how you lock your filing cabinets, and what security rules your employees must follow. This is security in the cloud. Your provider handles the infrastructure, but you still have to configure the settings, manage user permissions, and train your team properly.
What happens if the provider has an outage or a natural disaster strikes their data center? A potential partner's answer to this question says a lot about their operational maturity. A truly prepared provider will have a well-documented and regularly tested disaster recovery and business continuity plan.
This plan ensures that even in a worst-case scenario, your data can be restored quickly and securely, minimizing downtime and disruption to patient care.
Ask them for details on their backup frequency, data center redundancy, and their guaranteed recovery time objectives.
Choosing a provider is more than a simple transaction. While many services are fine for general business, finding the right hipaa compliant cloud storage demands a focused and critical eye. For smaller practices weighing their options, understanding these differences is vital. Our guide on the top cloud storage for small business offers more context on the features that matter most.
In the end, partnering with a provider who shows a deep commitment to security, transparency, and shared responsibility is the only way to protect your patients, your practice, and your own peace of mind.
The days of paper charts tucked away in filing cabinets are quickly becoming a memory. Today's healthcare is swimming in a sea of data, thanks to the boom in electronic health records (EHRs), telehealth platforms, and the ever-growing number of patient-worn health devices. This isn't just a small change; it’s a seismic shift in how patient care is managed.
This digital transformation means healthcare organizations are creating and handling more data than ever before. Every virtual consultation, every updated patient record, and every reading from a heart monitor adds to this massive flow of information. Suddenly, the need for scalable, secure storage isn't a future problem—it's an immediate operational must-have.
The sheer volume of this data is staggering, and it brings both incredible opportunities and serious risks. While all this information can lead to better patient outcomes and more efficient operations, it also creates a much larger target for cybercriminals. Each data point is a potential weak spot if it isn't properly protected.
This reality has shifted HIPAA-compliant cloud storage from a "nice-to-have" luxury to an essential piece of modern healthcare infrastructure. Trying to manage this explosion of data on local, on-premise servers is often inefficient, expensive, and a real headache to secure against today's sophisticated threats.
The responsibility on healthcare providers is immense. Failing to adopt secure, compliant storage is no longer just a compliance risk—it’s a direct barrier to future-proofing your practice in an increasingly interconnected world of patient care.
You don't have to take my word for it—just follow the money. The global healthcare data storage market is expanding rapidly as organizations scramble to keep up with these new digital demands. In fact, the market, valued at USD 6.28 billion in 2025, is projected to nearly triple to USD 20.98 billion by 2034. You can explore the full analysis of the healthcare data storage market trends on Precedence Research.
This surge isn't just about storing files; it's about building a foundation for the future of healthcare. It’s driven by the need to support telehealth, analyze data from wearables, and deliver personalized medicine—all of which depend on having a secure and accessible place for ePHI to live. A robust international keyword strategy can help providers connect with diverse patient populations, ensuring that localized content on health matters is both secure and accessible.
This growth also highlights a critical point: as the volume of data grows, so does the responsibility. A modern practice must have a storage solution that can scale with its needs while maintaining the highest security standards. Effectively managing these growing digital files is a core part of patient safety, and you can learn more about this by reviewing best practices for cloud asset management.
At the end of the day, secure cloud storage is no longer optional because the very nature of healthcare has changed. It's the engine that powers modern medical services, the vault that protects patient trust, and the framework that enables future innovation. Embracing it isn't just about compliance; it's about ensuring your practice can thrive securely in a digital-first world.

Staying compliant isn't a one-and-done achievement; it's a moving target. As cyber threats get smarter, the technology we use to protect electronic Protected Health Information (ePHI) has to evolve even faster. What was once considered a cutting-edge feature is quickly becoming the new baseline, so keeping an eye on these trends is crucial for the long-term safety of patient data.
The future of HIPAA compliant cloud storage is all about moving from a reactive to a proactive and intelligent security model. Staying ahead of the curve means embracing these next-generation tools before they become mandatory. This includes considering technical SEO for international reach to ensure that your security information and services are discoverable by a global audience.
Two key technologies have moved from "nice-to-have" to "must-have" for protecting ePHI from breaches and accidental leaks: Multi-Factor Authentication (MFA) and Data Loss Prevention (DLP).
Adopting these tools is a fundamental step in modernizing your security. If you're planning this kind of transition, our cloud migration checklist offers a helpful framework for a smooth and secure move.
Looking beyond today’s best practices, emerging tech like blockchain is on the verge of providing a whole new level of data integrity. While most people associate it with cryptocurrency, the core idea is powerfully simple for healthcare.
Imagine a digital logbook where every single action—every time a file is viewed, changed, or shared—is recorded as a permanent, unchangeable "block" in a chain.
Blockchain technology creates a tamper-proof audit trail for ePHI. Because each entry is cryptographically linked to the previous one, it becomes virtually impossible for anyone to alter historical records without detection, providing the ultimate proof of data integrity.
This creates a transparent and unbreakable record of who did what and when, completely changing how we verify the authenticity of patient data. For global organizations, conversion optimization per region becomes critical, ensuring that security features are not only robust but also clearly communicated on geo-targeted landing pages to build trust and drive adoption.
The global cloud storage market, valued at USD 43.6 billion in 2024, is set to expand at a 21.5% CAGR through 2034. As more healthcare providers move to the cloud, features like MFA and DLP are becoming non-negotiable. At the same time, innovations like blockchain, with its own massive expected growth rate of 53.6%, are preparing to add another powerful layer of decentralized, transparent security.
The bottom line is that the goalposts for security are always moving. Leading HIPAA compliant cloud storage providers like Sky Drive Folder are constantly innovating to stay ahead of these challenges, ensuring your patient data remains protected not just today, but for whatever comes next.
Picking a provider is just the first step. True HIPAA compliance isn't a one-time setup; it's an ongoing commitment. Once you've partnered with a HIPAA compliant cloud storage service, the real work of building a culture of security begins—a daily process of vigilance, training, and constant improvement.
Protecting patient data depends on having a practical, daily playbook. It means moving beyond the initial agreement and actively embedding secure practices into your organization's DNA. This playbook should cover all aspects of digital outreach, including how multilingual assets are handled and what content types that drive global conversions are approved for use.
A successful rollout starts with a clear plan. The goal is to turn abstract compliance rules into concrete actions your team can follow every single day. This playbook should be a living document, one you update as your practice evolves and new threats pop up.
Here are the essential steps to get started:
Establish Strict User Access Controls: Right away, you need to implement the "principle of least privilege." This is a simple but powerful idea: every user should only have access to the absolute minimum information they need to do their job. A receptionist, for example, has no reason to see the same detailed patient records as a physician.
Develop a Robust Training Program: Compliance is a team sport. Every single employee, from the front desk to senior medical staff, must be trained on your security policies, why protecting ePHI is so critical, and how to spot potential threats like phishing emails.
Create a Clear Incident Response Plan: Don't wait for a data breach to figure out what to do. You need a detailed incident response plan before you need it. This plan should spell out the exact steps to take, who to notify, and how to contain the damage and inform affected individuals, ensuring you can respond swiftly and without panic.
A critical part of this is performing regular risk assessments. This isn't a task you do once and forget about. It's a recurring process—at least annually—where you actively hunt for vulnerabilities in your systems, processes, and even your vendor's security to find and fix weak points before they can be exploited.
Maintaining compliance requires consistent effort. It's all about turning best practices into daily habits so that protecting patient data becomes second nature to your entire team. For global practices, this also includes a strategy for backlink building in target regions to establish authority and trust in local markets.
To help, here is a practical checklist for keeping your security posture strong:
Ultimately, achieving and maintaining compliance with a solution like Sky Drive Folder is a partnership. The provider secures the infrastructure, but it's your organization that builds and maintains the culture of security that keeps patient data safe, day in and day out.
When you're wading into the world of HIPAA compliant cloud storage, a lot of practical questions pop up. It's a complex topic, so let's clear up some of the most common points of confusion healthcare providers run into.
No, they definitely are not. The free, standard versions of these services are for personal use and don't meet HIPAA's strict requirements.
To use them for electronic Protected Health Information (ePHI), you have to subscribe to a specific business-level plan, like Google Workspace or Dropbox Business. But here's the most critical part: you must sign a Business Associate Agreement (BAA) with them. Without that signed contract, you are not compliant, period.
A Business Associate Agreement is the legal cornerstone of your vendor relationships. It’s a contract required by HIPAA between a healthcare provider (the Covered Entity) and any third-party service that touches your ePHI (the Business Associate).
This document spells out exactly how the vendor will protect your data, what they're allowed to do with it, and makes them legally responsible for any data breaches on their end.
Think of a BAA as the legal handshake that makes your partnership official under HIPAA. Using any cloud service to store, process, or transmit patient data without a signed BAA is a direct violation and one of the first things auditors look for.
Not automatically, and this is a misconception that gets a lot of practices into trouble. HIPAA compliance works on what’s called a shared responsibility model.
Your provider handles the security of the cloud—things like their physical data centers, the network infrastructure, and server hardware. That’s their half.
Your organization, however, is still 100% responsible for security in the cloud. This is your half, and it includes crucial duties like:
A compliant provider is a non-negotiable part of the puzzle, but it’s only one part. Your own internal policies and how you use the service are just as important.
Ready to secure your data with a solution built for compliance and peace of mind? Discover how Sky Drive Folder can simplify your file management while upholding the highest security standards. Learn more and get started today.